
A landmark clinical trial published in 2015, called the Learning Early About Peanut Allergy (LEAP), showed that the introduction of peanut products into the diets of infants at high risk of developing peanut allergy was safe. This led to an 81% reduction in the subsequent development of the peanut allergy. Prior to 2008, clinical practice guidelines recommended avoidance of potentially allergenic foods in the diets of young children who were at heightened risk for the development of food allergies. The LEAP study was the first to show that the early introduction of dietary peanut is actually beneficial.
An extension of the LEAP study published in 2016 called the Learning Early About Peanut Allergy – On (LEAP-On) demonstrated that regular consumption of peanut-containing foods beginning in infancy induces peanut tolerance that persists following a year of avoidance. This suggests that there are lasting benefits of early-life consumption for infants at high risk for developing peanut allergy. Investigators found that most children from the original peanut-consumption group remained protected from peanut allergy at age 6.
A new study called the Learning Early About Peanut Allergy – Trio (LEAP-Trio), sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), and published in the journal NEJM Evidence on May 28, 2024, further revealed that feeding children peanut products regularly from infancy to age 5 years of age reduced the rate of peanut allergy in adolescence by 71%, even when the children ate or avoided peanut products as desired for many years.
The LEAP investigators designed the LEAP-Trio study in order to test whether the protection gained from early consumption of peanut products would last into adolescence if the children could choose to eat peanut products in whatever amount and frequency they desired. The study team enrolled 508 of the original 640 LEAP trial participants—nearly 80%—into the LEAP-Trio study. 255 participants had been in the LEAP peanut-consumption group and 253 had been in the LEAP peanut-avoidance group.
The adolescents were assessed for peanut allergy primarily through an oral food challenge. This oral food challenge involved giving participants gradually increasing amounts of peanut in a carefully controlled setting to determine if they could safely consume at least 5 grams of peanut, the equivalent of more than 20 peanuts.
The study found that 15.4% of the participants from the early childhood peanut-avoidance group and 4.4% of the individuals from the early childhood peanut-consumption group had peanut allergy at age 12 or older. These results showed that regular, early peanut consumption reduced the risk of peanut allergy in adolescence by 71% compared to early peanut avoidance.
The study team also discovered that although participants in the LEAP peanut-consumption group ate more peanut products throughout childhood than the other participants overall, the frequency and amount of peanut consumed varied widely in both groups and included periods of not eating peanut products. This demonstrated that the protective effect of early peanut consumption lasted without the need to eat peanut products consistently throughout childhood and early adolescence.
These results confirm that feeding young children peanut products beginning in infancy can provide lasting protection from peanut allergy and further reinforce the current guidelines about the benefits of the early introduction of peanut products.
Despite the research about the early introduction of peanuts in infants, it is very important that every parent or guardian discuss this with their infant’s pediatrician before introducing peanuts to their child. Parents and guardians should follow their pediatrician’s recommendation and also seek care from a board certified allergist for an allergy consultation.
The board certified allergy specialists at Black & Kletz Allergy have been diagnosing and treating food allergies for more than 50 years. We treat both adult and pediatric patients. Black & Kletz Allergy has offices in Washington, DC, McLean, VA (Tysons Corner, VA), and Manassas, VA. All 3 of our offices have on-site parking. For further convenience, our Washington, DC and McLean, VA offices are Metro accessible. Our McLean office location offers a complementary shuttle that runs between our office and the Spring Hill metro station on the silver line. For an appointment, please call our office or alternatively, you can click Request an Appointment and we will respond within 24 hours by the next business day. If you suffer from food allergies, we are here to help you sort out whether or not you actually have an allergy vs. a food sensitivity. Our allergists will educate you on what to look for and what to do going forward regarding your specific food allergies. Black & Kletz Allergy is dedicated to providing the highest quality allergy care in a relaxed, considerate, and professional environment.


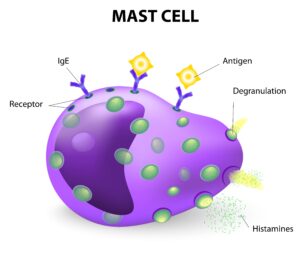 Mast cells are types of white blood cells that generally are found in the connective tissues. There are granules inside the mast cells that contain chemical mediators such as histamine, heparin, tryptase, prostaglandins, leukotrienes, serotonin, and cytokines. Many of these mediators are inflammatory in nature. In addition, mast cells have the allergy antibody, known as IgE, attached to their surfaces. Mast cells play an important role in initiating and promoting immune responses to pathogens (i.e., bacteria, viruses) and toxins (i.e., mold, flying insect stings) by releasing these chemical mediators Mast cells are also responsible for immediate allergic reactions. In an allergic reaction, the IgE on the surface of the mast cells bind to the proteins (i.e., allergens) that cause allergies. The mast cell is now activated, which causes the granules and their contents to be extruded from the mast cells into the tissues in a process called degranulation. As a result, the chemical mediators, which include histamine and chemicals that cause inflammation, are released into the tissues. These chemicals cause the typical symptoms that are generally associated with allergies such as
Mast cells are types of white blood cells that generally are found in the connective tissues. There are granules inside the mast cells that contain chemical mediators such as histamine, heparin, tryptase, prostaglandins, leukotrienes, serotonin, and cytokines. Many of these mediators are inflammatory in nature. In addition, mast cells have the allergy antibody, known as IgE, attached to their surfaces. Mast cells play an important role in initiating and promoting immune responses to pathogens (i.e., bacteria, viruses) and toxins (i.e., mold, flying insect stings) by releasing these chemical mediators Mast cells are also responsible for immediate allergic reactions. In an allergic reaction, the IgE on the surface of the mast cells bind to the proteins (i.e., allergens) that cause allergies. The mast cell is now activated, which causes the granules and their contents to be extruded from the mast cells into the tissues in a process called degranulation. As a result, the chemical mediators, which include histamine and chemicals that cause inflammation, are released into the tissues. These chemicals cause the typical symptoms that are generally associated with allergies such as  It is that time of the year again. Soon you will be seeing children (and some adults) trick or treating in your neighborhood searching for candy. For children, Halloween is a time to be with their friends, eat a lot of candy, and dress in scary costumes. For millions of parents however, Halloween can also be scary, but for a different reason: Their children have food allergies. According to Food Allergy Research & Education (FARE), approximately 6 million or 1 in 13 children in the U.S. have food allergies. This is about 8% of the U.S. pediatric population which is equivalent to about 2 children per classroom. In addition, more than 26 million adults also have food allergies. Together, there are about 32 million individuals with food allergies in the U.S. which is approximately 10% of the population. What is even more frightening is that the food allergy prevalence among children has increased dramatically within the last 30 years.
It is that time of the year again. Soon you will be seeing children (and some adults) trick or treating in your neighborhood searching for candy. For children, Halloween is a time to be with their friends, eat a lot of candy, and dress in scary costumes. For millions of parents however, Halloween can also be scary, but for a different reason: Their children have food allergies. According to Food Allergy Research & Education (FARE), approximately 6 million or 1 in 13 children in the U.S. have food allergies. This is about 8% of the U.S. pediatric population which is equivalent to about 2 children per classroom. In addition, more than 26 million adults also have food allergies. Together, there are about 32 million individuals with food allergies in the U.S. which is approximately 10% of the population. What is even more frightening is that the food allergy prevalence among children has increased dramatically within the last 30 years. Immunizations are one of the most effective and safe ways of preventing or reducing the risk of serious illness from various infections. Vaccinations also prevent infections from spreading from one individual to another, thus protecting the health and well-being of the general population. One should always check with one’s primary care provider before getting a vaccine. The CDC recommends vaccines for adults based on a variety of factors which may include age, travel destinations, sexual activity, health history, occupation, lifestyle, and previous vaccinations. The CDC currently recommends the following immunizations:
Immunizations are one of the most effective and safe ways of preventing or reducing the risk of serious illness from various infections. Vaccinations also prevent infections from spreading from one individual to another, thus protecting the health and well-being of the general population. One should always check with one’s primary care provider before getting a vaccine. The CDC recommends vaccines for adults based on a variety of factors which may include age, travel destinations, sexual activity, health history, occupation, lifestyle, and previous vaccinations. The CDC currently recommends the following immunizations: In children with milk allergy, the immune system falsely identifies the protein in the milk as potentially dangerous, and as a result, mounts a defensive attack. The “pre-formed” milk specific antibodies (i.e., immunoglobulin E or IgE) react with the protein in the milk (i.e., antigen), causing release of chemical substances (e.g., histamine, leukotrienes, prostaglandins) into the tissues. These chemical substances are what causes the symptoms of allergic reactions. Cow’s milk is the most common cause of milk allergy although milk from sheep and goats can also cause allergic reactions in certain sensitized children. Children are more likely to have a milk allergy if there is a history of a food allergy in other family members.
In children with milk allergy, the immune system falsely identifies the protein in the milk as potentially dangerous, and as a result, mounts a defensive attack. The “pre-formed” milk specific antibodies (i.e., immunoglobulin E or IgE) react with the protein in the milk (i.e., antigen), causing release of chemical substances (e.g., histamine, leukotrienes, prostaglandins) into the tissues. These chemical substances are what causes the symptoms of allergic reactions. Cow’s milk is the most common cause of milk allergy although milk from sheep and goats can also cause allergic reactions in certain sensitized children. Children are more likely to have a milk allergy if there is a history of a food allergy in other family members. Generalized itching (i.e., generalized pruritus) is a condition which can be quite annoying. It is when an individual has diffuse itching of the body usually without an associated rash. Approximately 20-25% of the general population experiences generalized pruritus at least one time in their life. The itching may be intermittent or it may be chronic in nature. “Acute” itching is when the itching has been present for less than 6 weeks. “Chronic” itching is defined by having it for 6 or more weeks. The itching may last for years in certain individuals. The severity of the itching may vary from very mild to very severe where it can interfere with one’s quality of life. If the itching becomes chronic, it is important to see a
Generalized itching (i.e., generalized pruritus) is a condition which can be quite annoying. It is when an individual has diffuse itching of the body usually without an associated rash. Approximately 20-25% of the general population experiences generalized pruritus at least one time in their life. The itching may be intermittent or it may be chronic in nature. “Acute” itching is when the itching has been present for less than 6 weeks. “Chronic” itching is defined by having it for 6 or more weeks. The itching may last for years in certain individuals. The severity of the itching may vary from very mild to very severe where it can interfere with one’s quality of life. If the itching becomes chronic, it is important to see a  Anaphylaxis is an acute, severe, and life-threatening allergic reaction. The most common triggers for anaphylaxis include allergenic foods, medications, and insect stings. Symptoms usually begin within a few minutes of exposure of the triggering agents. Initially, the symptoms characteristically involve the skin which typically causes itching and hives followed by swelling of the soft tissues. Unless treated, the reaction may rapidly progress and may involve other organ systems (e.g., respiratory, gastrointestinal, cardiovascular) resulting in symptoms such as shortness of breath, wheezing, coughing, nausea, vomiting, abdominal pain, dizziness, drop in blood pressure, and/or loss of consciousness.
Anaphylaxis is an acute, severe, and life-threatening allergic reaction. The most common triggers for anaphylaxis include allergenic foods, medications, and insect stings. Symptoms usually begin within a few minutes of exposure of the triggering agents. Initially, the symptoms characteristically involve the skin which typically causes itching and hives followed by swelling of the soft tissues. Unless treated, the reaction may rapidly progress and may involve other organ systems (e.g., respiratory, gastrointestinal, cardiovascular) resulting in symptoms such as shortness of breath, wheezing, coughing, nausea, vomiting, abdominal pain, dizziness, drop in blood pressure, and/or loss of consciousness. As the Summer marches on and we are now in the month of August, many allergy sufferers are about to get ready for another foe, namely ragweed. Usually about August 15th of every year, ragweed pollen begins to blanket the
As the Summer marches on and we are now in the month of August, many allergy sufferers are about to get ready for another foe, namely ragweed. Usually about August 15th of every year, ragweed pollen begins to blanket the  Contact dermatitis
Contact dermatitis Now that it is Summer, mosquitoes are becoming more prevalent in the Washington, DC, Northern Virginia, and Maryland region. Mosquitoes are flying insects that tend to be more widespread where there is standing water. They are more active early in the morning and early in the evening. Female mosquitoes typically lay their eggs in stagnant water. Only the female mosquito bites and feeds on human blood, as they need this blood in order to produce their eggs. Male mosquitoes, on the other hand, feed on water and nectar. Mosquitoes are considered pests and they are a nuisance to almost everyone who comes in contact with these annoying insects. When a person is bitten, the mosquito injects its saliva into the skin which contains proteins that prevent the human blood from clotting. This allows the blood to be transferred to the mosquito’s mouth without clotting. For the most part, mosquitoes bite people and animals without any symptoms or only very mild local symptoms. For many others however, a mosquito bite can cause a great deal of misery, mostly consisting of irritation, itching, redness, and/or swelling at the site of the bite. In very sensitive individuals, the swelling and redness can become quite large. Occasionally this redness and swelling is accompanied by bruising and/or blisters.
Now that it is Summer, mosquitoes are becoming more prevalent in the Washington, DC, Northern Virginia, and Maryland region. Mosquitoes are flying insects that tend to be more widespread where there is standing water. They are more active early in the morning and early in the evening. Female mosquitoes typically lay their eggs in stagnant water. Only the female mosquito bites and feeds on human blood, as they need this blood in order to produce their eggs. Male mosquitoes, on the other hand, feed on water and nectar. Mosquitoes are considered pests and they are a nuisance to almost everyone who comes in contact with these annoying insects. When a person is bitten, the mosquito injects its saliva into the skin which contains proteins that prevent the human blood from clotting. This allows the blood to be transferred to the mosquito’s mouth without clotting. For the most part, mosquitoes bite people and animals without any symptoms or only very mild local symptoms. For many others however, a mosquito bite can cause a great deal of misery, mostly consisting of irritation, itching, redness, and/or swelling at the site of the bite. In very sensitive individuals, the swelling and redness can become quite large. Occasionally this redness and swelling is accompanied by bruising and/or blisters. Grass pollen allergy is a very common environmental allergy. Grass pollinates in at different time of the year depending on where in the U.S. one is located. In the Northeastern and Mid-Atlantic regions of the U.S., grass pollinates from the Spring through the Summer. In the
Grass pollen allergy is a very common environmental allergy. Grass pollinates in at different time of the year depending on where in the U.S. one is located. In the Northeastern and Mid-Atlantic regions of the U.S., grass pollinates from the Spring through the Summer. In the  In order to understand conjunctivitis, one must first understand a little about the anatomy of the eye as well as a little physiology of the way eyes become lubricated. The conjunctiva is the thin transparent membrane that lines the inside of the eyelids (i.e., palpebral area) and the front of the eyeballs (i.e., bulbar area). The lacrimal glands, which are located in the outer corners of the eyes, secrete tears which lubricate the eyes. These tears then drain into the nose via tear ducts from the inner corners of the eyes. Inflammation of the conjunctival membrane is called conjunctivitis. There are several conditions which cause inflammation of the conjunctiva which are as follows:
In order to understand conjunctivitis, one must first understand a little about the anatomy of the eye as well as a little physiology of the way eyes become lubricated. The conjunctiva is the thin transparent membrane that lines the inside of the eyelids (i.e., palpebral area) and the front of the eyeballs (i.e., bulbar area). The lacrimal glands, which are located in the outer corners of the eyes, secrete tears which lubricate the eyes. These tears then drain into the nose via tear ducts from the inner corners of the eyes. Inflammation of the conjunctival membrane is called conjunctivitis. There are several conditions which cause inflammation of the conjunctiva which are as follows: Summertime in the metropolitan
Summertime in the metropolitan  The symptoms of asthma may include a feeling of chest tightness or heaviness in the chest, wheezing (i.e., high-pitched whistling type of noise during breathing), coughing, and/or shortness of breath/difficulty in breathing. The frequency of these symptoms varies depending on the severity of the asthma. The symptoms can be intermittent or persistent. The severity is also classified as either mild, moderate, or severe. Asthma usually begins in childhood, although it can also be diagnosed for the first time in adulthood. The course of asthma is variable. The symptoms can be mild, moderate, severe, frequent, infrequent, intermittent, and/or persistent at various times throughout one’s life.
The symptoms of asthma may include a feeling of chest tightness or heaviness in the chest, wheezing (i.e., high-pitched whistling type of noise during breathing), coughing, and/or shortness of breath/difficulty in breathing. The frequency of these symptoms varies depending on the severity of the asthma. The symptoms can be intermittent or persistent. The severity is also classified as either mild, moderate, or severe. Asthma usually begins in childhood, although it can also be diagnosed for the first time in adulthood. The course of asthma is variable. The symptoms can be mild, moderate, severe, frequent, infrequent, intermittent, and/or persistent at various times throughout one’s life. As we enter into Spring, not only should allergy-sensitive individuals be on the lookout for those annoying pollen allergy symptoms, but they should be aware of their surroundings for venomous flying insects. In the Washington, DC, Maryland, and Northern Virginia metropolitan area, the most common venomous flying insects are honey bees, wasps, yellow jackets, white-faced hornets, and yellow-faced hornets. The summer months are the peak months that insect stings occur. In the U.S., about 3% of the population experience allergic reactions to the venom of flying insect stings. Approximately a half a million individuals seek emergency room care every year for insect sting reactions in the U.S. Unfortunately, there are roughly 50 deaths reported each year from these insect sting reactions.
As we enter into Spring, not only should allergy-sensitive individuals be on the lookout for those annoying pollen allergy symptoms, but they should be aware of their surroundings for venomous flying insects. In the Washington, DC, Maryland, and Northern Virginia metropolitan area, the most common venomous flying insects are honey bees, wasps, yellow jackets, white-faced hornets, and yellow-faced hornets. The summer months are the peak months that insect stings occur. In the U.S., about 3% of the population experience allergic reactions to the venom of flying insect stings. Approximately a half a million individuals seek emergency room care every year for insect sting reactions in the U.S. Unfortunately, there are roughly 50 deaths reported each year from these insect sting reactions.









